ATTENTION PATIENTS:
Beware of scammers claiming to be from a Ballad physician office calling about new Medicare cards. Do not share personal information. If you believe you have received a fraudulent call, please report it to the FTC at ReportFraud.ftc.gov. If you ever question a call from Ballad Health, please hang up and call your physician's office or 833-8-BALLAD directly.
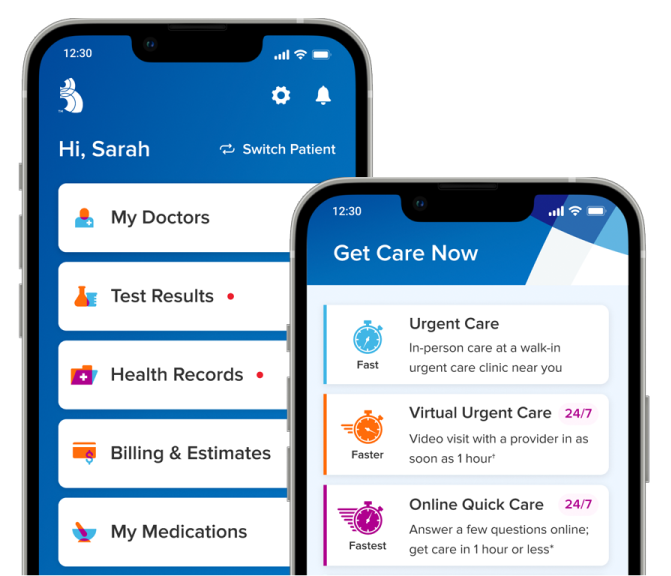
Find the best urgent care option for you
Answer a few online questions & receive feedback in 1 hour (pending volume)
No appointment
No video needed
$30 flat fee
Video visit with a Ballad Health urgent care provider in as soon as 1 hour
Appointment needed
Video needed
$49 or billable to insurance
For minor injuries or everyday illnesses – all without a costly trip to the ER
Walk-ins welcome
Save wait time – book ahead online
Self-pay & most insurance accepted

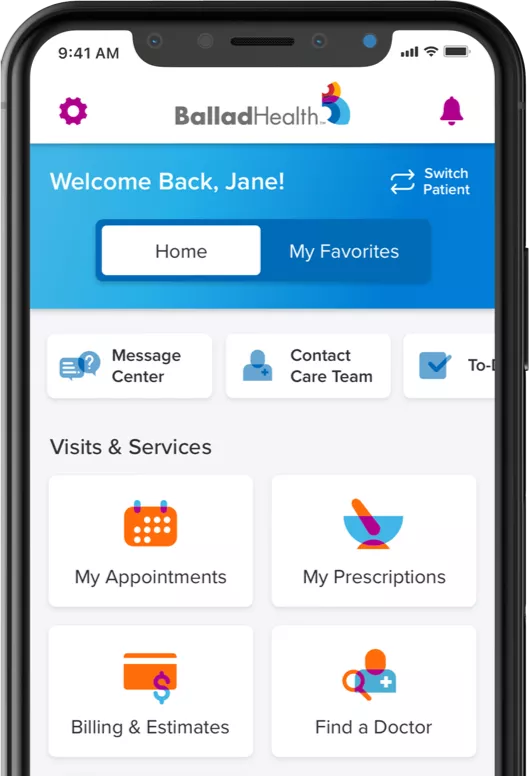
Ballad Health was created to improve the health and well-being of those we serve, and we plan to honor your trust by providing you and your family the highest quality care possible.
We know you want a healthcare provider who truly listens to you and understands what you need.
Investing in Appalachia
At Ballad Health, we're completely dedicated to the success of our region because we're your neighbors – and this is our community too.
Re-imagining rural healthcare